Menopausal issues can seem like an overwhelming, confusing subject. It’s possible that you’re suffering from hot flashes of sweat, night sweats, or mood swings, and are wondering what options you have. The most common term refers to “hormone therapy,” an approach that usually comes with a mix of strong opinions and contradicting information. The subject has been a source of controversy, which has left people unsure of which side to take.
Let’s get this out of the way. Let’s look at what menopausal hormone therapy is expected to look like by 2025. This article will help you understand the most recent thinking that will help you discern fact from fiction and be more secure in your health options. We’ll discuss how the discussion has changed and what contemporary alternatives are available to you.
A Brief Look Back: Why Was Hormone Therapy So Controversial?
To know where we are now, it’s beneficial to understand the past. For a long time, the hormone therapy (HRT), which is now often referred to as menopausal hormonal therapy (MHT), was the most commonly used treatment for menopausal symptoms. Then, in the beginning of the 2000s, a significant research study known as”the Women’s Health Initiative (WHI) published findings that linked hormone therapy to a higher risk for health problems, including heart disease and breast cancer.
Thus, anxiety and confusion quickly spread. The number of prescriptions for HRT decreased in the meantime, and doctors as well as patients began to be cautious. This study changed the discussion around menopausal treatments for years.
But the understanding of medicine has advanced since then. Scientists have taken a close review of the initial WHI study and also conducted their own studies. The preliminary conclusions weren’t the entire truth. The research mainly focused on postmenopausal and older women and utilized specific types of hormones, which differ from the many choices that are available today. The risks that were identified did not apply to everyone, particularly not women who began therapy at the end of their 40s or in their early 50s.

The medical profession today has a more balanced approach. We are now aware that for a lot of people, the advantages of hormone therapy far outweigh the risks, particularly if it is initiated at the appropriate time.
Hormone Therapy in 2025: What’s New and Different?
The method of menopausal hormone therapy has evolved to be more customized. There is no longer a standard prescription that is universally applicable. Instead, your doctor will collaborate with you to create an appropriate solution that is tailored to the specific health conditions, symptoms, background, and preferences.
Personalized and Lower-Dose Options
A significant shift coming to 2025 will be focusing on using the smallest effective dose in the least amount of duration. This strategy maximizes benefits while minimizing risk. The doctor will not just give you a generic medication. They will take into consideration your specific situation.
For example, if your main complaint is dryness of the vagina, it is possible to be prescribed a low-dose local estrogen product such as a ring, cream tablet, or cream. These products can work on the area where they’re required, and do not affect your entire body. However, if you’re suffering from general symptoms such as night sweats and hot flashes, it could be time to seek treatments that circulate in the bloodstream, like patches, gels, or pills.
The Rise of Body-Identical Hormones
Another major advancement is the growing use of hormones that have a body-identical structure. They are derived from plants and are structurally similar to the hormones that your body produces naturally, including progesterone and estradiol. A lot of women and their doctors favor these hormones since they are believed to be a better fit for the body.
For instance, progesterone that is micronized progesterone is frequently preferred over synthetic progestins in older ages, due to its better safety profile, specifically with the risk of breast cancer and its effects on mood. In the same way, transdermal estrogen (delivered via a gel or patch) is a popular first-line treatment option since it bypasses the liver, thus reducing the chance of blood clots, compared with oral estrogen.
Focusing on Quality of Life and Long-Term Health
The debate about hormone therapy isn’t only about controlling hot flashes anymore. It’s also about maintaining your health over time and ensuring you have a good quality of life. We’ve learned that the decrease in estrogen in menopausal women can impact more than just body temperature.
For instance, estrogen plays a crucial role in maintaining bone density. Hormone therapy can greatly lower your risk of developing osteoporosis and fractures later on in your life. Additionally, it can assist with other less well-known ailments such as headaches, joint pain, and sleep disturbance. In addressing these issues, MHT makes to feel more comfortable and is a huge benefit.
Who Is a Good Candidate for Hormone Therapy?
Based on the latest research on who is to be a suitable potential candidate to undergo MHT by 2025? Most often, healthy women suffering from uncomfortable menopausal symptoms and who are younger than sixty (or less than 10 years from their last menstrual cycle) are excellent candidates.
But it’s not appropriate for all. It’s not usually advised if you have a background of:
- Breast cancer and other cancers
- Vaginal bleeding that is not explained
- Heart attack, blood clots, stroke, or heart attack
- Liver disease
The decision to commence the hormone therapy is deeply personal. It requires a lengthy conversation with a medical professional who is well-versed in the most recent research on menopausal symptoms. Together, you’ll be able to evaluate your personal signs, your medical background, and risk factors to make a well-informed decision.

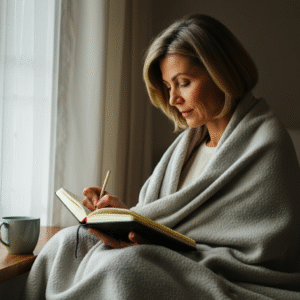
Menopausal hormonal therapy can be overwhelming. However, you don’t have to go through it all on your own. The most important thing is to have updated, current information, and to find a dependable doctor.
Begin by recording your symptoms. A journal will aid you in having a more productive discussion with your doctor. Do not be afraid to ask questions. Find out about the various kinds of hormones, the delivery methods (patch gel, pill, or patch), and the specific advantages and risks that apply to you.
The ultimate goal is to boost your well-being through this natural transition. Through continuing research and a more precise approach to treatment, hormone therapy will be a safe and effective way to ease the burden for many women by 2025. The fear-based era is over, and a fresh emphasis on personalization, clarity, and empowerment has been replaced.